Ever noticed a dark blue or black spot forming on your arm or legs after a fall? While most people dismiss the common injury, sometimes the spot could be more than a small bruise: a bruise occurs because of damage to a small blood vessel(s), but when a larger blood vessel gets damaged, it could lead to a hematoma.
A hematoma is the collection of blood outside a large blood vessel. Hematomas usually occur after the wall of a blood vessel (artery, vein, or capillary) gets damaged and the blood leaks into the surrounding tissue. Unlike a haemorrhage in which the bleeding does not stop, however, the blood gets clotted in a hematoma.
A hematoma can be small (just a dot of blood) or it can be large and can cause significant damage. Our body can take care of damage caused by minor injuries: whenever there is damage to the vessel wall, the body starts repairing it by activating the blood clotting agents and starts forming fibrin patches. But when the damage is extensive, the body is unable to repair it and the defect keeps on bleeding. This allows some hematomas to expand with time.
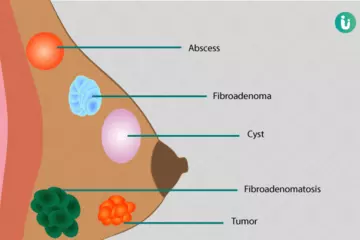
The blood that leaks from the damaged blood vessels causes inflammation, pain, swelling, and redness in the surrounding tissue. Hematomas may occur anywhere in the body but their symptoms depend upon their location, size and the underlying reason for the hematoma.
While most hematomas resolve on their own, some—especially those hematomas that are not visible to the naked eye—may require urgent medical attention. Hematomas can be dangerous for those who are on blood thinners (anticoagulants) or have any blood clotting disease.