Summary
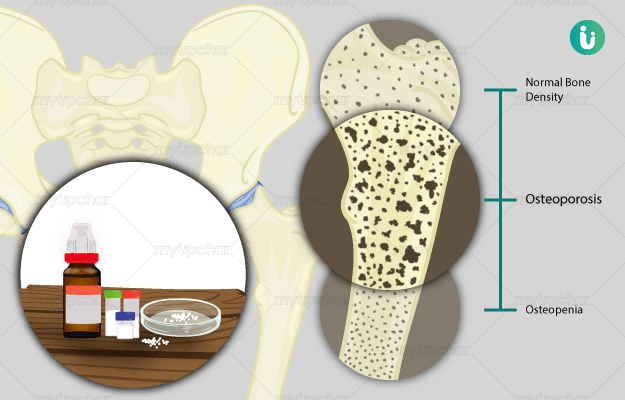
Osteoporosis is a condition of the bones in which the bones lose their density and start to become brittle. This weakening of the bone and the resulting complications are more common in women than in men.The most common causes of osteoporosis include menopause leading to hormonal changes, deficiency of calcium and Vitamin D, and the presence of other diseases which could cause weakening of the bones. The biggest health risk for people with osteoporosis is fractures from injuries and falls. It is common for people with osteoporosis to have weakened bones and also a poor posture from curved bones. Hormone therapy, dietary supplements and healthy lifestyle form the mainstay of treatment. When diagnosed early, bones can be protected from further damaged and risk of fractures can be minimized.

 Doctors for Osteoporosis
Doctors for Osteoporosis  OTC Medicines for Osteoporosis
OTC Medicines for Osteoporosis
 Osteoporosis articles
Osteoporosis articles News for Osteoporosis
News for Osteoporosis

 Ayurvedic Treatment of Osteoporosis
Ayurvedic Treatment of Osteoporosis
 Diet for Osteoporosis
Diet for Osteoporosis
 Home Remedies for Osteoporosis
Home Remedies for Osteoporosis
 Homeopathic Treatment of Osteoporosis
Homeopathic Treatment of Osteoporosis





































 Editorial Team
Editorial Team



 Dt. Akanksha Mishra
Dt. Akanksha Mishra

 Dr. Rachita Narsaria
Dr. Rachita Narsaria