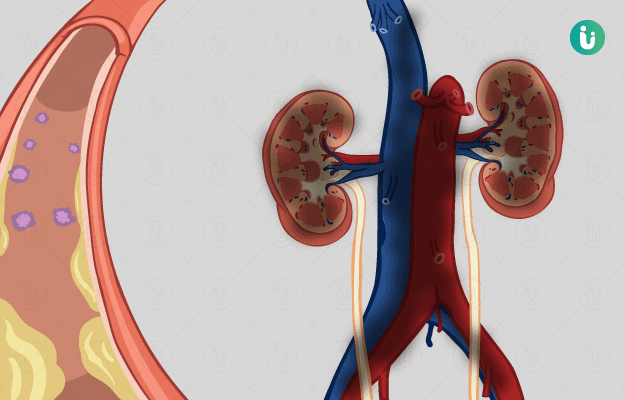
Uremia refers to raised blood levels of protein and amino acid metabolism end products, urea and creatinine. Usually, these metabolic toxins are expelled in the urine by kidneys. Rising levels of urea and creatinine indicate kidney dysfunction. Azotaemia is the term given to a high blood urea nitrogen (BUN) level that is not severe enough to produce symptoms. Uremia commonly sets in due to chronic end-stage renal disease (ESRD) but can also arise in acute kidney injury. End-stage renal disease is the last stage of chronic kidney disease (CKD), as classified by the falling glomerular filtration rate (GFR), indicating a value of kidney function less than 15%. Estimated glomerular filtration rate (eGFR) is a clinical indicator calculated on the basis of blood creatinine level and indicates how well the glomeruli (basic filtration unit in the kidney composed of a tuft of blood vessels bringing in and taking away toxic waste) are functioning to filter blood. The manifestations of uremia can affect the neurological, cardiovascular, endocrine, gastrointestinal, skeletal, skin and immune systems. It can also impact the blood and nutritional status of the individual. Undiagnosed and untreated uremia can prove fatal.
Bumper Offer - Urjas oil Just @ Rs. 1
X

- हिं - हिंदी
- En - English
 Doctors for Uremia
Doctors for Uremia  OTC Medicines for Uremia
OTC Medicines for Uremia