Summary
Colporrhaphy is a surgery recommended in women with pelvic organ prolapse. In this condition, the supporting tissues that hold the pelvic organs (uterus, urinary bladder, etc.) in their original position become weak. This leads to the bulging of the pelvic organs into the wall of the vagina, which causes pain or discomfort in the vagina, difficulty in controlling urine, and affects sexual life. Colporrhaphy involves repairing the supporting tissues between the vagina and pelvic organs with strong stitches. It helps to hold the pelvic organs back in their original position and provides relief from the symptoms of pelvic organ prolapse. The operation lasts for around 90 minutes, and you will be hospitalised for about one to two days after the surgery. You will have a follow-up appointment after two to three weeks of surgery to review your condition.
- What is colporrhaphy?
- Why is colporrhaphy recommended?
- Who can and cannot get colporrhaphy?
- What preparations are needed before colporrhaphy?
- How is colporrhaphy done?
- How to care for yourself after colporrhaphy?
- What are the possible complications/risks of colporrhaphy?
- When to follow up with your doctor after a colporrhaphy?
What is colporrhaphy?
Colporrhaphy is a surgical procedure to repair the vaginal wall in women with pelvic organ prolapse, a condition in which the organs in the pelvis bulge out into the vagina.
Pelvic organs including the uterus (womb), bladder, and bowel are held in position inside the body with muscle fibres and ligaments (bands of elastic, tough tissue). However, certain conditions like childbirth, obesity, or long-term constipation can weaken these supporting tissues. In such a scenario, these tissues will not be able to hold the pelvic organs in their original position, resulting in the bulging of the pelvic organs into the vagina and causing pain and discomfort. This condition is called pelvic organ prolapse. Types of pelvic organ prolapse are as follows:
- Rectocele: Bulging or prolapse of the rectum into the back of the vaginal wall.
- Cystocele: Prolapse of the urinary bladder into the front wall of the vagina.
- Uterine prolapse: The uterus prolapses into the upper part of the vagina.
- Vaginal vault prolapse: Bulging of the upper part of the vagina after the uterus removal surgery.
Pelvic organ prolapse does not pose a risk to your life. If the condition causes mild symptoms, your healthcare consultant will recommend lifestyle changes such as preventing constipation and losing weight to treat the condition. However, if it causes severe symptoms that affect your day-to-day activities, surgery will be recommended. Colporrhaphy is one such surgery that involves repairing the weakened supporting tissues with stitches to put the prolapsed organs back in their original position. Depending on the procedure, colporrhaphy is divided into two types, namely anterior (to repair the front vaginal wall) and posterior colporrhaphy (to repair the back vaginal wall).
Why is colporrhaphy recommended?
This procedure is recommended in women with pelvic organ prolapse. The following symptoms are associated with this condition:
- A feeling of a bulge inside the vagina or coming out of the vaginal wall
- Difficulty urinating
- Involuntary leaking of urine
- An urge to urinate frequently
- A discomfort or dragging sensation inside the vagina
- A feeling of heaviness around the genitals and lower abdomen
- Backache
- A feeling of numbness or discomfort during sex
What preparations are needed before colporrhaphy?
You may be asked to visit the hospital a few days before the surgery for a preoperative assessment. It helps to determine if you need any special care before or after the surgery and whether you have any health issues that need treatment before you undergo the surgery. The surgeon will ask you about your health, medical history, and conduct an internal pelvic examination. Besides, you will also be asked to get a few blood and urine tests done. Your doctor may ask you:
- For a list of all medications that you take, including herbs and over-the-counter medicines.
- To stop taking blood-thinning medicines such as ibuprofen, aspirin, and warfarin.
- If you have a history of any allergies including an allergy to anaesthesia medicines.
- To avoid smoking.
- Whether you are pregnant.
- To remove all the body piercings, make-up, and nail polish, and take a bath before arriving at the hospital on the scheduled day of the surgery.
- To arrange for a friend, family member, or responsible adult to drive you home after your discharge from the hospital.
- To inform him/her if you develop a cold, fever, or flu on the days leading to the surgery.
- To not drink or eat anything after midnight of the night prior to the surgery.
- To sign a consent form allowing him/her to perform the procedure.
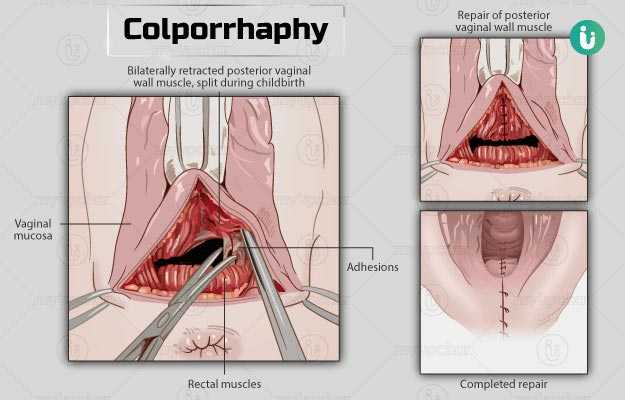
How is colporrhaphy done?
After you arrive at the hospital, the hospital staff will ask you to wear a hospital gown. They will then start an intravenous (IV) line in your arm or hand to supply fluids and medications during the surgery. A urinary catheter (a thin tube) will also be placed inside your bladder to drain urine.
The procedure usually involves the following:
- An anaesthetist will give you general anaesthesia to keep you relaxed and asleep during the surgery.
- Someone from the surgery team will remove your pubic hair.
- The surgeon will then make a cut on the front or back wall of your vagina based on the position of the prolapse.
- He/she will repair the supporting tissue between the vaginal wall and the prolapsed organ using strong stitches.
- Then, the surgeon will close the incision on your vaginal wall with stitches and place a vaginal pack (like a rolled-up bandage) in your vagina to stop the bleeding.
The surgery lasts for around 90 minutes. The stitches used in the procedure are typically dissolvable and, therefore, need not be removed. You will need to stay in the hospital for about one to two days after the surgery and expect the following during your hospitalisation:
- You will be encouraged to walk once you regain consciousness after the surgery. The hospital staff will provide you with compression stockings to prevent the formation of blood clots.
- You may have to take some medications to relieve pain following the surgery.
- There may be some drainage and bleeding from your vagina. You will be provided with sanitary napkins to help absorb it.
- The urinary catheter will be removed on the day after the surgery.
- You will be asked to take a liquid diet for a few days after the surgery. You will be allowed to resume a solid diet as soon as your bowel function improves.
How to care for yourself after colporrhaphy?
Once you reach home, you will need to take care of yourself in the following manner:
- The surgeon will prescribe pain medications and laxatives to help control your pain and allow regular bowel movements, respectively. Take the medicines as directed.
- You can take a shower as usual. However, the doctor may suggest you clean the outside of your vagina with soap and water twice a day. Take care that the soap water does not go inside your vagina.
- You can resume your daily activities in about six weeks.
- Take short walks during the initial two weeks. However, avoid lifting objects that weigh over 5 kg during this period. You can gradually increase your activities after two weeks.
- You will experience slight bleeding for the first two weeks. Sanitary napkins may help with it. Do not use tampons unless your surgeon allows you to.
- You will be allowed to drive about two weeks after the surgery.
- Avoid activities that can contribute to the recurrence of pelvic organ prolapse such as smoking and standing for extended periods of time.
- You can resume your sexual life six weeks after the surgery.
When to see the doctor?
Contact the doctor if you experience any of the following:
- Difficulty breathing
- Chest pain
- Heavy bleeding from the vagina
- Pain, redness or swelling in the legs
- Temperature above 100.4°F (38°C)
- Redness, hotness or bleeding at the incision site
- Inability to urinate
- Nausea or vomiting
- Blood in urine or cloudy urine
- The urge to urinate frequently
- Pain while urinating
What are the possible complications/risks of colporrhaphy?
The possible risks and complications associated with the surgery include:
- Excessive bleeding that might require a blood transfusion
- Damage to other pelvic organs
- Bladder injury
- Mild pain in the buttocks
- Damage to any particular nerve due to your position during the surgery
- Formation of a blood clot in legs or lungs
- Obstruction in the bowel, resulting in bloating, abdominal pain, nausea or vomiting
- Urinary tract infection
- Discomfort during sexual activity
- Formation of thicker (scar) tissue at the operated site
- Recurrence of pelvic organ prolapse
- Problems with urination such as leaking of urine or the inability to empty the bladder
When to follow up with your doctor after a colporrhaphy?
The surgeon will ask you to visit the hospital two to three weeks after surgery to review your progress.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Royal Berkshire Hospital [Internet]. NHS Foundation Trust. National Health Service. UK; Surgical repair of vaginal prolapse
- National Health Service [Internet]. UK; Pelvic organ prolapse
- Michigan Medicine [internet]. University of Michigan. US; Repair of Vaginal Wall Prolapse (Vaginal Vault Prolapse)
- Hernandez A, Sherwood ER. Anesthesiology principles, pain management, and conscious sedation. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 14.
- Miller RD, ed. Miller's Anesthesia. 8th ed. Philadelphia, PA: Elsevier Saunders; 2019
- University College London Hospitals [Internet]. NHS Foundation Trust. National Health Service. UK; Colporrhaphy
- Walters MD, Karram MM, eds. Urogynecology and Reconstructive Pelvic Surgery. 4th ed. Philadelphia, PA: Elsevier Saunders; 2015
- Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017
- Wein AJ, Kavoussi LR, Partin AW, Peters CA, eds. Campbell-Walsh Urology. 11th ed. Philadelphia, PA: Elsevier; 2016