Summary
A craniotomy is performed to remove a part of the skull bone (bone flap) for a brain surgery. The bone flap may be removed from the eyebrow region, the cheek and eye socket area or behind the hairline or ear. A computed tomography (CT) scan, magnetic resonance imaging (MRI) or endoscope are used to help locate the area to be treated. The bone flap may be put back again after the surgery. However, sometimes, the bone flap is removed permanently.
Before the surgery, the healthcare practitioner will perform a physical examination and conduct various diagnostic tests to check if you are in good health and hence fit enough to undergo the surgery. The operation may require sedatives and anaesthesia. After the surgery, the incision area should be kept clean and dry. Avoid putting pressure on the head, bending over the waist or lifting heavy objects for a few weeks after the surgery.
Craniotomy helps in improving the symptoms related to various brain conditions.
- What is craniotomy?
- Why is a craniotomy recommended?
- Who can and cannot get a craniotomy?
- What preparations are needed before a craniotomy?
- How Is Craniotomy Done?
- How to care for yourself after craniotomy?
- What are the possible complications/risks of craniotomy?
- When to Follow Up With Your Doctor?
What is craniotomy?
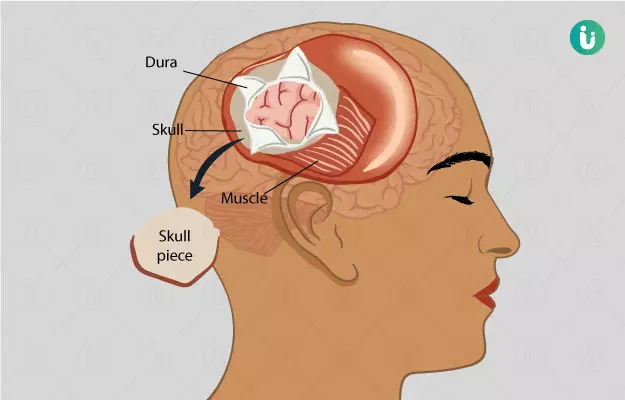
A craniotomy is a surgical procedure to remove a part of the skull bone to allow access to the brain underneath.
The skull consists of 22 bones. It protects our brain and supports the soft tissues within the skull (intracranial soft tissues). A section of the skull bone called the bone flap is removed using specialized tools. After the surgery, the flap is attached again using small titanium plates and screws.
Why is a craniotomy recommended?
A craniotomy is required for multiple conditions. Some of the conditions and the symptoms associated with these conditions are:
Brain aneurysm (ballooning of a blood vessel in the brain):
- Drooping eyelids
- Blurred vision or double vision
- Confusion
- Seizures
- Stiff neck
- Weakness or numbness
- Pain above and behind the eyes
- Sudden severe headaches
- Nausea or vomiting
- Dilated pupil
Brain tumour:
- Hearing loss
- Unexplained, frequent vomiting
- Problems in reasoning
- Headache that worsens on coughing, exercise or when changing positions
- Memory loss
- Speech difficulties
- Behavioural and personality changes
- Gradual loss of sensation or movement in the leg or arm
Hydrocephalus (fluid build-up in the hollow places inside the brain):
- Slowed development
- Poor appetite
- Eyes that stay looking down
- Tiredness
- Vomiting
- Fussiness
Who can and cannot get a craniotomy?
Healthcare practitioners perform this surgery for the following reasons:
- Repair or clipping of an aneurysm
- Repair of a skull fracture
- Diagnosis, removal or treatment of a brain tumour/tumours
- Repair of a tear in the membrane lining of the brain (dura mater)
- For treating epilepsy
- Relieving intracranial pressure (pressure inside the brain)
- Implantation of a stimulator device in the brain. These devices are used to treat movement disorders like dystonia and Parkinson’s
- To stop bleeding or remove blood clot from a leaky blood vessel
- Treatment for hydrocephalus
Craniotomy has no rigid contraindications; however, it can be avoided in the following conditions as they increase the risks associated with this surgery:
- Severe cardiopulmonary disease
- Poor functional status
- Advanced age (elderly)
- Severe systemic collapse (sepsis and multiorgan failure)
What preparations are needed before a craniotomy?
- Before the surgery, you will be asked to sign a consent form. This form grants permission for the surgery and anaesthesia.
- The healthcare practitioner will do a comprehensive physical examination, including blood tests and diagnostic tests, to ensure that you are fit for the surgery.
- A neurological examination is also performed to compare with the test results after surgery.
- Inform your healthcare practitioner if:
- If you smoke, the healthcare practitioner will ask you to stop smoking to improve your chances of speedy recovery after the surgery.
- Fasting is required for the surgery. Your doctor would inform you for how long.
- You may be given sedatives to help relax before the surgery.
- The night before the surgery, you may be asked to use an antiseptic shampoo to wash your hair.
How Is Craniotomy Done?
The following steps are performed during the surgery:
- The healthcare provider will ask you to remove your clothes, jewellery or any item that interferes with the surgical procedure. You will have to wear a gown provided by the hospital for the surgery.
- A urine catheter will be inserted into your bladder to collect urine and empty your bladder and an intravenous (IV) line will be placed in your arm or hand to provide you with necessary fluids and medicines.
- Your heart rate, breathing, oxygen level and blood pressure will be continuously monitored during the surgery.
- To begin the surgery, excess hairs would be shaved off from the site of the surgery and it will be cleaned with an antiseptic solution.
- You will be given general anaesthesia for the surgery.
- To get your head into the right position for the surgery, a healthcare practitioner will secure your head in a specialised holder device, such as a Mayfield three-pin head holder. The device may be attached to the operating table already.
- Next, the surgeon will make an incision on the skin of your skull. The type of incision will be decided on the basis of the affected area and the type of craniotomy - a smaller incision is made in endoscopy craniotomy.
- After the incision, the surgeon will then part or pull up your scalp.
- To control bleeding caused due to the incision, he/she will place a surgical clip on your scalp.
- Next, A medical drill and saw will be used to make burr holes and cut the bone in your skull, respectively.
- The surgeon will then remove and save the bone flap.
- The dura mater will be detached from the bone and cut to expose the brain.
- Depending on the condition, the surgeon will further monitor and perform the surgery. For example, a monitor will be placed inside the brain tissue to check the pressure inside the brain.
- After the surgery is done, the layers will be sewed (sutured) together.
- The bone flap will be attached again using plates, suture or wires.
- The scalp will be closed with suture or surgical staple.
- Next, the area will be covered with sterile bandage or dressing.
Some types of craniotomy are as follows:
- Craniectomy: In this type of surgery, the bone flap is not replaced immediately. After a few weeks or months, the removed part is replaced using a metal plate, synthetic material or the person’s original bone. In some cases, the bone flap portion is removed permanently.
- Image-guided craniotomy or stereotactic craniotomy: This surgery is performed using a computer and various imaging procedures, such as magnetic resonance imaging (MRI) or computed tomography (CT) scan. The three-dimensional images help to locate the exact area in the brain that is to be treated.
- Endoscopy craniotomy: In this surgery, an endoscope is used to visualize the area in the brain. It involves the insertion of a lighted scope with a camera through a small hole in the skull.
- Minimally invasive supra-orbital craniotomy: This type of surgery involves an incision (cut) within the eyebrow region. It causes lesser pain, minimizes scarring and enables speedy recovery.
- Orbitozygomatic craniotomy: This surgery includes temporary removal of the bone from the cheek and the eye socket (orbit) area. It gives better access to the brain and minimizes brain damage.
- Extended bifrontal craniotomy: In this surgery, an incision is made behind the hairline.
- Translabyrinthine craniotomy: In this surgery, the bone behind the ear is removed. This surgery may cause permanent hearing loss.
- Retro-sigmoid ‘keyhole’ craniotomy: In this surgery, an incision is made behind the ear. It minimizes pain and scarring and improves recovery.
After the surgery
After the surgery is performed, you will be shifted to a recovery room and then to the intensive care unit (ICU). In the ICU, your head will be kept raised to prevent brain swelling, and your intracranial pressure will be monitored. The healthcare practitioner will give you medicines to lessen your brain swelling.
Gradually, the devices used to measure intracranial pressure will be removed. Once you are stable, you will be shifted to your hospital room. You will still have the urinary catheter and oxygen support for a few more days or till your discharge. This support will be taken off too before you are discharged.
To prevent pneumonia, you will be taught deep-breathing exercises to get back your lung function.
Your brain function will be checked by asking you some questions to check your awareness level, checking your pupil and asking you to move your arms and legs.
Based on your condition after surgery, your diet may vary. Liquids are usually given a few hours after surgery, and you are gradually transitioned to more solid foods as you start to tolerate them.
When you are able to, you will be asked to walk around a bit. A physical therapist will initially help you with this. Once you are able to walk, the urine catheter would be removed too. Inform your doctor if you have any symptoms of urine infection once the catheter is removed. The physical therapist will check your balance, movements and strength. You may be shifted to a rehabilitation facility till you regain your strength or the therapist will suggest some exercises to regain your strength.
Before discharge from the hospital, the healthcare practitioner will give you instructions for home care and arrange your follow-up meetings.
How to care for yourself after craniotomy?
Even after you are at home, you may experience:
- Itching, pain, burning and numbness at the surgical site
- Clicking sound as the bones slowly reattach; these bones may take six to 12 months to heal completely
- Small amount of fluid under the incision skin
- Worsening of swelling in the morning when you wake up
- Headaches especially when you cough, deep breath or are active
- Fatigue
Medications:
- Your doctor may prescribe certain medicines, such as antibiotics or pain killers for you to take at home.
- Obey all the instructions given by the doctor while taking medicines and don’t skip any dose.
Diet and activities:
- Unless advised by the healthcare practitioner, you can follow your regular diet.
- You should increase your activities slowly.
- Use hand railings while walking on stairways.
- Avoid lifting anything heavy for the first two months after the surgery.
- Do not put pressure on your head or bend over your waist.
- Consult your healthcare practitioner to know when you can have sex or begin driving again.
Wound care:
- Keep the area of the incision clean and dry.
- Wear a shower cap when you bathe until the staple or stitches are removed.
- After the stitches are removed, rinse and wash your incision and pat dry.
- Change your bandage if it is wet or dirty.
- Wear a loose hat or turban. Avoid the use of a wig for three to four weeks.
- Avoid using any hair product with harsh chemical, cream or lotion on the incision area.
- Wrap ice in a towel and place it on the surgical site to reduce swelling or pain. You should sleep with the head raised on the pillows.
A craniotomy can help in improving the symptoms related to a brain condition. These symptoms may be headache, seizures or paralysis in a limb due to brain tumour.
When to See the Doctor?
Call your healthcare practitioner if you observe the following symptoms:
- Fever
- Increased pain around the surgical site
- Confusion
- Seizure
- Speech problems
- Green, yellow or blood-tinged sputum
- Weakness in arms or legs
- Swelling, redness, drainage or bleeding around the incision site or face
What are the possible complications/risks of craniotomy?
Some of the possible risks of craniotomy are as follows:
- Brain swelling
- Haematoma (blood clot)
- Temporary or permanent neurological deficit (stroke)
- Infection
- Fits
- Leakage of fluid from around the brain (cerebral spinal fluid)
- Heart attack
- Pneumonia
- Pulmonary embolism (clot from the legs passing to the lungs)
- Urinary tract infection
- Deep vein thrombosis (clots in the legs)
When to Follow Up With Your Doctor?
You will have a follow-up meeting with your healthcare practitioner at six to eight weeks after the surgery. During the follow-up visit, stitches and surgical staples will be removed. Also, your doctor will inform you about further follow-up visits.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- University of Rochester Medical Center [Internet]. Rochester (NY): University of Rochester Medical Center; Craniotomy
- Oncolink [Internet]. Philadelphia: Trustees of the University of Pennsylvania; c2018. Surgical Procedures: Craniotomy
- John Hopkins All Children's Hospital [Internet]. Johns Hopkins Medicine. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Craniotomy
- Brain Aneurysm Foundation [Internet]. Massachusetts. US; Brain Aneurysm Basics
- Zaky W, Ater JL, Khatua S. Brain tumors in childhood. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 524.
- Kieran MW, Chi SN, Manley PE, et al. Tumors of the brain and spinal cord. In: Orkin SH, Fisher DE, Ginsburg D, Look AT, Lux SE, Nathan DG, eds. Nathan and Oski's Hematology and Oncology of Infancy and Childhood. 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 57.
- National Cancer Institute [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Childhood Brain and Spinal Cord Tumors Treatment Overview (PDQ®)–Health Professional Version
- Nemours Children’s Health System [Internet]. Jacksonville (FL): The Nemours Foundation; c2017; Hydrocephalus
- Winn H Richard. Youmans Neurological Surgery. 6th Ed. Philadelphia: Elsevier; 2011.
- Sawyer MM. Postanesthetic care. In: Duke JC, Keech BM, eds. Anesthesia Secrets. 5th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 28.
- Ortega-Barnett J, Mohanty A, Desai SK, Patterson JT. Neurosurgery. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 67.
- University Hospital Southampton [Internet]. NHS Foundation Trust. National Health Service. U.K. Craniotomy
- Children's Health Queensland Hospital and Health Service [Internet]. Queensland Government. Australia; What is a craniotomy?