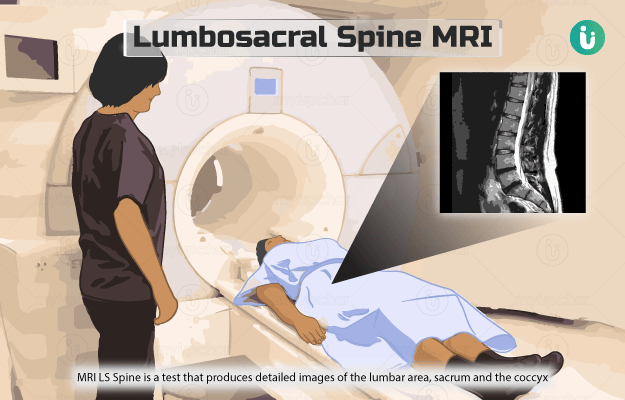
What is a Lumbosacral (LS) spine MRI?
Magnetic resonance imaging lumbosacral spine (MRI LS Spine) is a test that produces detailed images of the lumbar area (lower part of the spine), sacrum (base of the spine) and the coccyx (the tailbone). The test helps to identify or look for any problems in these areas of the spine.
Unlike an x-ray and CT scan machine, the MRI machine does not use any radiation. Instead, it uses a large magnet, radio waves and a computer for producing images of the internal structures of the body. During the scan, the magnets and radio waves align and realign the protons (parts of atoms) of the body in a particular way. This whole process is read by an attached computer, which uses the data to create images of the scanned area.
An MRI is sometimes done with a contrast dye, injected into the patient’s body right before the scan, The dye binds with body tissues and helps provide clearer images.