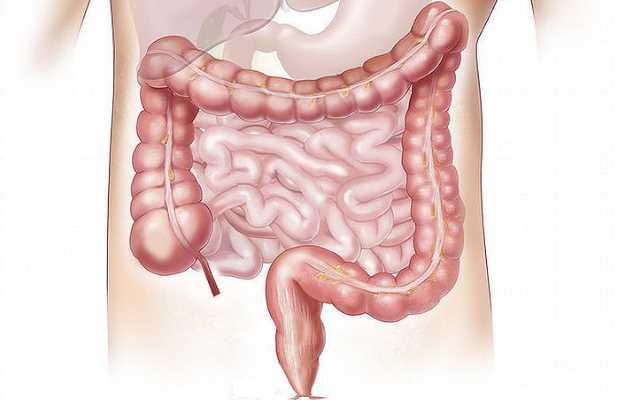
What is Gastrointestinal bleeding?
Gastrointestinal (GI) bleeding is a condition wherein there is a loss of blood from anywhere along the entire digestive tract, starting from the mouth to the anal opening. The bleeding can be acute and significant for a short duration or less severe but prolonged for years together.
What are its main associated signs and symptoms?
Gastrointestinal bleeding is broadly classified into upper gastrointestinal bleeding, which presents with symptoms, such as a vomit that is bright red in colour, vomit that looks like ground coffee, dark stools or blood mixed with stools; and lower gastrointestinal bleed with symptoms that include stools that are bright red in colour or bleeding from haemorrhoids associated with pain while passing stools. Signs and symptoms associated with chronic blood loss include fatigue, pale skin, anaemia, heart complications, nutritional deficiencies and collapse. Gastrointestinal bleeding has to be tackled at its earliest, as any blood loss can be life-threatening.
What are the main causes?
The causes of upper gastrointestinal bleed include
- Oesophageal varices.
- Stomach ulcers.
- Tears in the oesophageal lining called Mallory-Weiss syndrome.
- Oesophageal cancer.
A lower gastrointestinal bleed happens mainly from
- Duodenal ulcers.
- Crohn’s disease.
- Ulcerative colitis.
- Tumours.
- Haemorrhoids or piles.
- Anal fissures.
How is it diagnosed and treated?
A diagnosis is made by obtaining a detailed account of the person’s present and past medical history, thereby understanding the exact nature and pattern of the symptoms. This is followed by a thorough physical examination to look for the signs of bleeding.
Once this is done, a series of tests are ordered depending on the site of bleeding. In cases of upper gastrointestinal bleeding, an endoscopy is performed. This allows the doctor to visualise the upper gastrointestinal tract and look for any ulcers or varices. Similarly, to look for the causes of lower gastrointestinal bleeding, a colonoscopy is ordered. Other tests include a complete blood count, a stool test and an ECG, if required, depending on the age of the person.
Treatment depends on the cause. Medications to shrink blood vessels are administered. For peptic ulcers, proton pump inhibitors are given to reduce the production of stomach acid. Endoscopy also treats bleeding effectively by applying certain clips or bands to ligate the blood vessels. Supportive treatment includes blood transfusion, especially for significant blood loss. Haemorrhoids and rectal varices can be treated with surgery.

 OTC Medicines for Gastrointestinal Bleeding
OTC Medicines for Gastrointestinal Bleeding