Methicillin-resistant staphylococcus aureus (MRSA) has evolved over time into a bacterial strain distinct from staphylococcus aureus by accruing genetic changes that allow it to secrete chemicals that render beta-lactam antibiotics like penicillins and cephalosporins invalid. Some staphylococcus aureus strains that are found to be sensitive to methicillin are called methicillin-susceptible staphylococcus aureus (MSSA). There are three essential factors that contribute to MRSA infection.
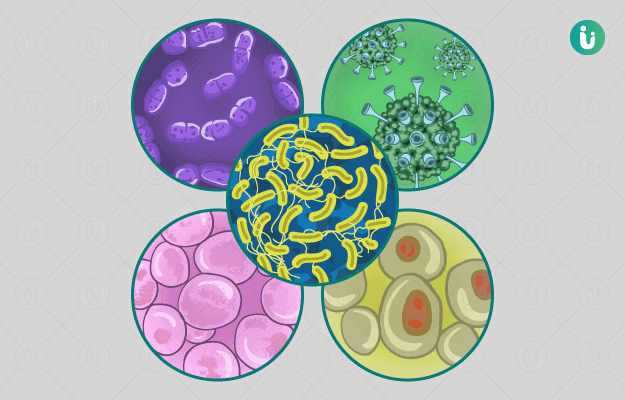
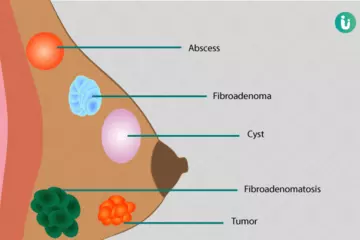
Staphylococcus aureus: Staphylococcus aureus is a round spherical shaped bacteria that usually appear in clusters upon viewing with a microscope and is Gram-positive, which means it changes colour with the application of reagent in Gram staining. Gram-positive bacteria have a thicker peptidoglycan outer cell wall but are generally more susceptible to treatment with antibiotics than Gram-negative bacteria. Staphylococcus aureus is a facultative anaerobic bacteria; it can thrive even without the presence of oxygen. Hence, it is a common causative organism of pyogenic, or pus-filled, infections and abscesses. Skin infections are the most common infections caused by staphylococcus aureus but, bloodstream infections, abscesses, osteomyelitis (bone infection), pneumonia and endocarditis are also possible. Of all the common infection-causing bacteria, staphylococcus aureus is perhaps the most feared due to its potential to cause widespread infection and its rising antibiotic resistance. Staphylococcus aureus is transmitted through touch and contact with a person infected with the bacteria whether the person displays symptoms of infection or not, as with an asymptomatic carrier. Due to this route of transmission, staphylococcus aureus infections can easily be spread in the community and hospital settings where sick patients can pass on the bacteria to other patients with compromised immune systems (for example, HIV patients, cancer patients, post organ transplant patients or patients receiving immunosuppressive treatment).
Methicillin: Penicillins are a class of antibiotics that share a similar chemical structure composed of one or more beta-lactam rings. Once a revolutionary drug that brought the modern world out of the pre-antibiotic era of preventable early deaths caused by minor infections, today penicillin is plagued by the problem of growing resistance towards it by bacteria. As a product of evolution, bacteria today have developed chemicals that can render some antibiotics ineffective against them; this is called antibiotic resistance. Many common infection-causing bacteria have developed the ability to secrete an enzyme called beta-lactamase, which breaks down the beta-lactam ring of penicillin and makes it inert. Methicillin is an antibiotic drug that works against certain bacteria and belongs to the class of Penicillins. Unlike other older generation penicillins, methicillin is resistant to the action of bacterial beta-lactamase, which means it can act on, and kill, the bacteria even if it secretes beta-lactamase. The beta-lactamase resistant property of methicillin made it a very important and effective last-resort antibiotic. Even though once it was effective against bacteria like streptococcus and staphylococcus, today the rising antibiotic resistance in bacteria has rendered methicillin ineffective in most cases. Thus, methicillin-resistant staphylococcus aureus (MRSA) gives rise to a two-fold problem – a commonly transmissible bacteria causing serious infections that have stopped responding to commonly available and highly effective antibiotics.
Antibiotic resistance: When antibiotics are used unsparingly and spuriously, the problem of antibiotic resistance arises. Bacteria respond to constant exposure to antibiotics by evolving and developing genes that award them defence mechanisms, like chemicals that can break down antibiotics and render them ineffective. Although evolution is an expected outcome in all organisms, this development is sped up by the use of unnecessary and excessive antibiotics to a rate that cannot keep pace with the production of new antibiotics. Incorrect diagnoses or prescription of antibiotics without sensitivity testing leads to increased use of incorrect antibiotics, which in turn may kill off bacteria in the body responsive to the antibiotic but allow resistant bacteria to persist, multiply and eventually be transmitted in the community. A common example of misguided use of antibiotics is its use to treat the common cold, which is, in fact, caused by a virus.
(Read more: Viral infections)

 Doctors for MRSA Infection
Doctors for MRSA Infection