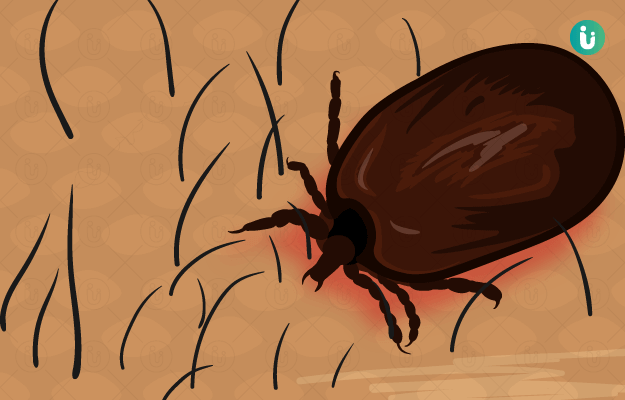
Scrub Typhus is a vector-borne disease spread by mite bites. The main cause of Scrub Typhus is rickettsia bacteria infection - rodents host the mites that carry this infection.
Up until the 1940s and 50s, Scrub Typhus was counted among lethal infectious diseases. Today, it can be brought under control with antibiotics like doxycycline and tetracycline. The challenge, however, is diagnosing it correctly because most symptoms of Scrub Typhus are non-specific.
The symptoms include fever, chills and rigors with a characteristic lesion known as eschar. The consulting doctor makes a diagnosis by recognising antibodies against the rickettsia bacteria in their blood, as well as taking evidential support from the eschar and other clinical features.
Cases of Scrub Typhus are more common during the rainy season and in hilly and forested areas. It is a serious public health problem in South-East Asia, North Australia and South Asia, including India. Globally, Scrub Typhus affects almost 1 million people every year.

 Doctors for Scrub Typhus
Doctors for Scrub Typhus