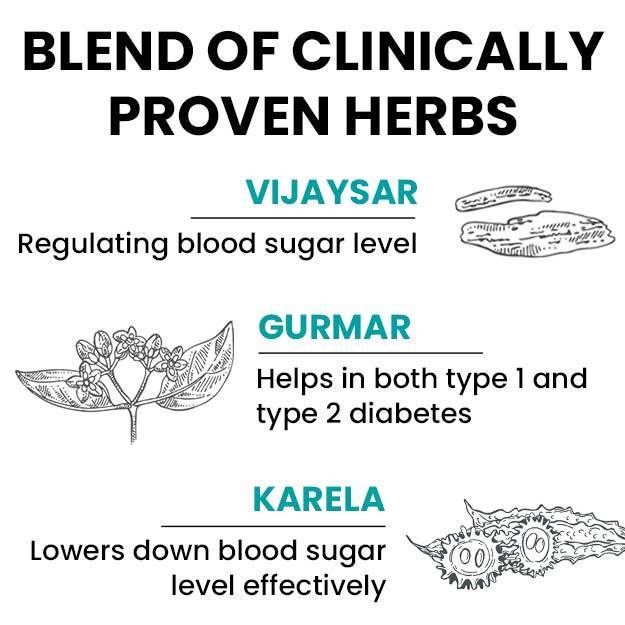
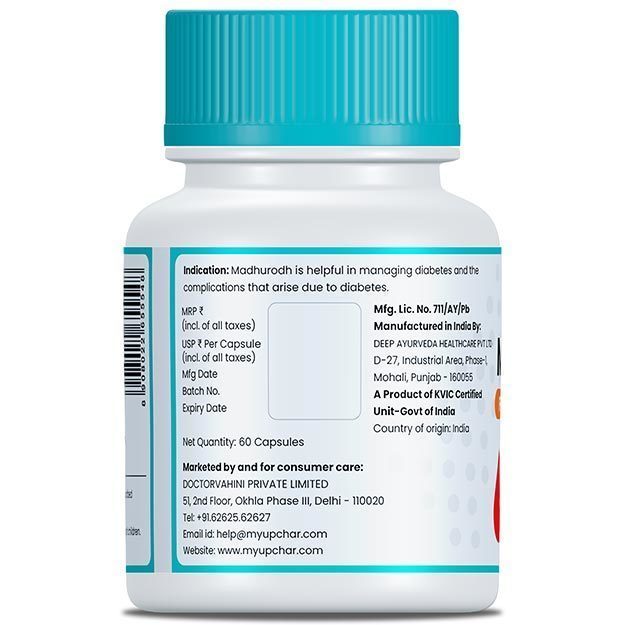
Hyperglycemia is the medical term used to describe an elevated or high blood level of glucose. Elevation of blood glucose can be transient or short-lived, as is the case after eating a meal, or associated with endocrine disorders affecting glucose metabolism of the body. The normal blood glucose level in healthy adults is less than 100mg/dL while on an empty stomach (i.e. upon waking in the morning after 8 hours or more of fasting, before breakfast) and less than 140 mg/dL two hours after eating a meal. Hyperglycemia is a commonly encountered problem in patients suffering from diabetes mellitus (type 1, type 2 and gestational diabetes mellitus) due to insulin deficiency and insulin resistance. Insulin is a hormone secreted by the beta islet cells in the pancreas and its action is metabolism and regulation of glucose uptake by cells of the body. Type 1 diabetes occurs due to an immune cell (autoantibody) mediated destruction of insulin-secreting cells; the resulting insulin deficiency inhibits the uptake of glucose by the body, leading to an increase in glucose circulating in the blood. Whereas in type 2 diabetes, insulin resistance develops generally due to poor lifestyle and obesity, inhibiting the hormone’s action on glucose blood levels. Gestational diabetes mellitus refers to the state of high blood glucose levels that develops in some pregnant women due to increased insulin resistance.
Click on the link to know in detail about the treatment of diabetes.
Although elevated blood glucose levels are pathognomonic of diabetes mellitus, usually with oral hypoglycemic agent (OHA) drugs like metformin and/or insulin, the blood glucose levels are maintained at the lowest possible levels for the patient. However, under some circumstances, like a skipped dose, a heavy meal or any other cause of acute stress on the body, blood glucose levels can rise uncontrollably. Diabetic ketoacidosis (DKA) and Hyperosmolar Hyperglycaemic Syndrome (HHS) are two dreaded complications of uncontrolled surges of blood glucose levels in diabetic patients. While diabetes mellitus is always associated with hyperglycemia, other non-diabetic conditions can also cause an abnormal increase in blood glucose levels.
(Read more: Diabetes in children)

 Doctors for Hyperglycemia (High blood sugar)
Doctors for Hyperglycemia (High blood sugar)  OTC Medicines for Hyperglycemia (High blood sugar)
OTC Medicines for Hyperglycemia (High blood sugar)
 Hyperglycemia (High blood sugar) articles
Hyperglycemia (High blood sugar) articles

















 Dr. Anurag Shahi (AIIMS)
Dr. Anurag Shahi (AIIMS)