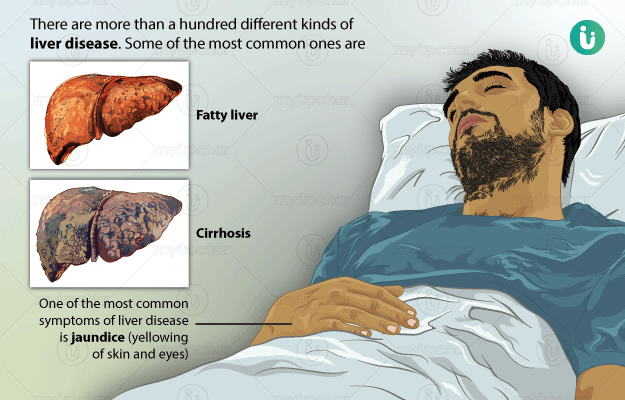
Alcoholic Liver Disease (ALD)
It is the most common liver disease and occurs due to excessive and regular alcohol intake. Alcohol acts as a poison to the liver and causes its inflammation. There is an accumulation of fat in the liver resulting in fatty liver. This fat accumulation affects liver functioning and causes symptoms like jaundice, nausea, vomiting, and enlarged veins in the food pipe (oesophageal varices). This eventually leads to irreversible damage to the liver called cirrhosis.
Non-alcoholic Steatohepatitis (NASH)
It is the second most common form of liver injury. The most common causes of NASH are obesity and uncontrolled diabetes, which result in injury to the liver cells and cause accumulation of fat in the liver cells. Symptoms of NASH are same as ALD, only the causes are different. If left untreated, it can result in liver cirrhosis and failure.
Viral Hepatitis
It is more common in developing countries. Infection by viruses, such as hepatitis A and hepatitis E results in acute liver injury. Hepatitis A and E infections are usually caused by eating food or beverages contaminated with these viruses. It results in jaundice, fever, nausea, vomiting, and abdominal pain. Infection with viruses like hepatitis B, hepatitis C, and hepatitis D can gradually damage the liver and cause chronic liver injury. These are blood-borne infections and spread through infected blood, use of infected needles-syringes, and sexual intercourse. Symptoms of viral liver infection appear gradually and present as slowly developing jaundice.
Hemochromatosis
It is one of the rare forms of metabolic liver disease where the body accumulates excess iron in the blood, as well as the liver. Iron accumulates in the liver cells damaging it and causing liver inflammation, cirrhosis, and eventually, liver failure or liver cancer if left untreated.
Primary Biliary Cholangitis
It is one of the rarest forms of liver disease, which is caused due to a faulty immune system that damages the bile ducts. The damaged bile ducts (small tubes that collect bile from liver cells) are unable to transport the bile to the gallbladder. Hence, these contents accumulate in the liver and damage the liver cells. If left untreated, it can lead to cirrhosis and eventually liver failure. This disease was earlier thus called as primary biliary cirrhosis.

 Doctors for Liver Disease
Doctors for Liver Disease  OTC Medicines for Liver Disease
OTC Medicines for Liver Disease
 Lab tests for Liver Disease
Lab tests for Liver Disease Liver Disease articles
Liver Disease articles
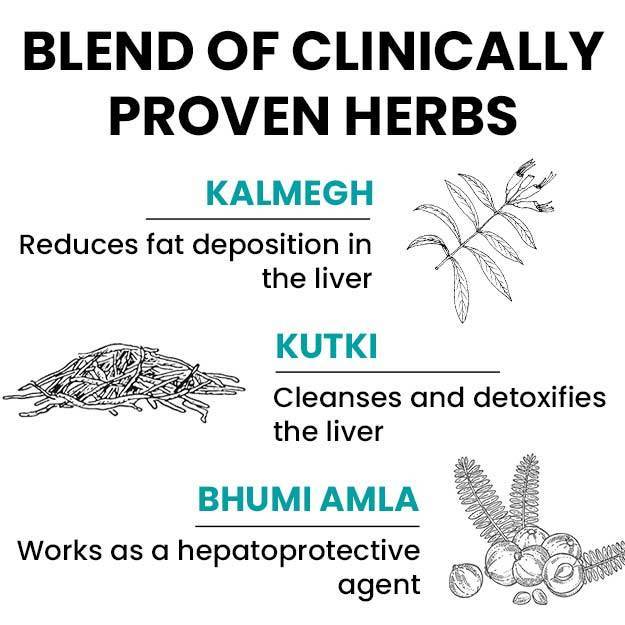
 Ayurvedic Treatment of Liver Disease
Ayurvedic Treatment of Liver Disease
 Homeopathic Treatment of Liver Disease
Homeopathic Treatment of Liver Disease















 Editorial Team
Editorial Team



 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla