It's time to talk about something many women experience but often feel shy to discuss: vaginal pain. If you've ever felt discomfort, burning, stinging, or any kind of ache down there, you're definitely not alone. This isn't a topic to suffer in silence over, and understanding it is the first step towards finding relief and getting back to feeling like yourself. Let's dive in and unravel this often-misunderstood issue.
- What Is Vaginal Pain?
- Causes Of Vaginal Pain
- Symptoms Of Vaginal Pain
- When Do Women Feel Vaginal Pain?
- Study Around Vaginal Pain
- How To Test For Vaginal Pain?
- How To Cure Vaginal Pain?
- Tablets For Vaginal Pain
- Home Remedies For Vaginal Pain
- Prognosis and complications
- Prevention of vaginal pain
- Summary
What Is Vaginal Pain?
So, what exactly are we talking about when we say "vaginal pain"? Simply put, it's any discomfort, soreness, burning, stinging, throbbing, or aching sensation felt in and around the vaginal area. This can range from mild irritation that's just a nuisance to severe, debilitating pain that affects daily life, intimacy, and overall well-being. It's not always a constant feeling; it might come and go, or only appear in specific situations. Think of it as your body's way of telling you something might be a little off, and it's worth listening to.
(Read More: Pubic Hair Removal: Safety Tips and Best Practices You Need)
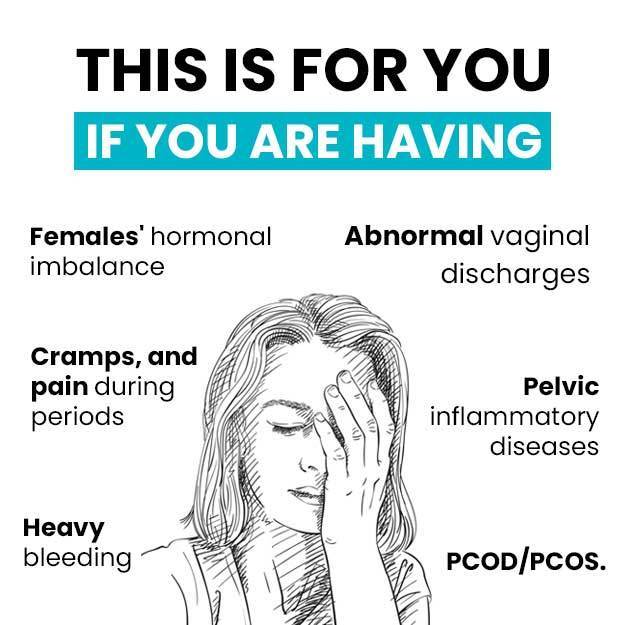
Causes Of Vaginal Pain
Vaginal pain can stem from a surprising number of sources, and it’s rarely just one thing. Often, it's like a puzzle with several pieces contributing to the whole picture. Some common culprits include infections, like yeast infections (which cause itching, burning, and discharge) or bacterial vaginosis (often leading to a fishy odor and discomfort). Sexually transmitted infections (STIs) can also be a cause, bringing symptoms like pain during sex or urination.
Here are some common categories of causes:
- Infections: Yeast infections, bacterial vaginosis, STIs.
- Skin Conditions: Eczema, psoriasis, lichen sclerosus affecting sensitive skin.
- Muscle Problems: Pelvic floor dysfunction, vaginismus (involuntary muscle clenching).
- Nerve Issues: Conditions like pudendal neuralgia.
- Hormonal Changes: Dryness and thinning of tissues during menopause or after childbirth.
- Psychological Factors: Stress, anxiety, or a history of trauma affecting muscle tension and pain perception.
(Read More: Beyond the Basics: Your Definitive Guide to the Copper T)
Beyond infections, skin conditions can play a role. Issues like eczema, psoriasis, or lichen sclerosus can affect the sensitive skin of the vulva and vagina, leading to dryness, itching, tearing, and pain. Muscle problems in the pelvic floor, which are the muscles that support your bladder, bowels, and uterus, can also cause significant pain. Conditions like vaginismus, where these muscles involuntarily clench, or pelvic floor dysfunction, where they are too tight or too weak, can make everyday activities and intimacy incredibly painful.
Sometimes, the pain is nerve-related. Conditions like pudendal neuralgia involve irritation or damage to the pudendal nerve, which supplies sensation to the pelvic area, leading to chronic burning or aching. Hormonal changes, particularly during menopause or after childbirth, can cause vaginal dryness and thinning of the tissues, known as atrophy, which can make the area very sensitive and prone to pain. Even psychological factors like stress, anxiety, or a history of trauma can contribute to or worsen vaginal pain by affecting muscle tension and pain perception. It's a complex area, and pinpointing the cause often requires a bit of detective work.
(Read More: Best Time To Get Pregnant)
Symptoms Of Vaginal Pain
The symptoms of vaginal pain are as varied as their causes, but generally, they involve some form of discomfort in the vaginal area. You might experience a burning sensation that feels like a constant fire, or a stinging feeling that intensifies with touch or movement. Some women describe it as a raw or chafed feeling, particularly after activity. It could be a persistent ache, a throbbing sensation, or even sharp, stabbing pains that come out of nowhere.
Common symptoms and sensations include:
- Burning
- Stinging
- Throbbing
- Aching
- Rawness or chafing
- Sharp or stabbing pains
- Itching, redness, swelling, or unusual discharge.
The pain might be localized, meaning it's in a very specific spot, or it could be diffuse, spreading across the entire vaginal and vulvar region. Sometimes, it's accompanied by itching, redness, swelling, or unusual discharge. For many, the pain is most noticeable during specific activities, such as sexual intercourse (dyspareunia), inserting tampons, or even just sitting for extended periods. It can also cause discomfort during urination or bowel movements. The key is to pay attention to how your body feels and when these sensations occur, as this information is invaluable in figuring out what's going on.
(Read More: Abortion: types, causes, pills, procedure, side effects)
When Do Women Feel Vaginal Pain?
Vaginal pain can pop up at various times, and recognizing these patterns can offer crucial clues. For many, it's most noticeable during sexual activity, whether it's during penetration or even just with touch. This pain can range from mild discomfort to severe, sharp pain, and it often impacts intimacy and relationships. It’s also common to experience pain during or after inserting a tampon, or during gynecological exams, which can make these necessary tasks feel daunting.
Here are some common scenarios when vaginal pain might be felt:
-
During or after sexual intercourse
-
When inserting tampons
-
During gynecological exams
-
During or after exercise
-
While sitting for extended periods
-
When wearing tight clothing
-
During urination or bowel movements
-
Spontaneously, without any obvious trigger
-
At specific times in the menstrual cycle
(Read More: When To Have Sex After Tubectomy?)
Simple daily activities like sitting for long periods, wearing tight clothing, or even just walking can trigger or worsen the pain for others. For some, the pain might be spontaneous, meaning it just appears without any obvious trigger, persisting throughout the day. It could also be tied to specific times in their menstrual cycle, changing with hormonal fluctuations. Understanding when the pain occurs helps both you and your doctor narrow down potential causes and find the right solutions.
Study Around Vaginal Pain
Chronic Vulvar and Gynecologic Pain: Prevalence and Characteristics in a Self-Reported Survey
The study, titled "Chronic Vulvar and Gynecologic Pain: Prevalence and Characteristics in a Self-Reported Survey," was authored by Gloria A Bachmann et al. It was published in the Journal of Reproductive Medicine in January 2006.
Key findings include that approximately 4% of participants reported experiencing vulvar pain within the six months prior to the survey, while 17% reported other forms of chronic gynecologic pain. Women who reported either vulvar or non-vulvar pain were twice as likely as asymptomatic women to have a history of depression and vaginal infections. They also reported a poorer quality of life and higher stress levels. Dyspareunia (painful intercourse) and pain during daily activities were more commonly reported by women with vulvar pain compared to those with non-vulvar gynecologic pain.
The study utilized a cross-sectional retrospective survey design. A questionnaire was distributed via mail to women aged 18 to 80 years who were ambulatory patients at an academic multidisciplinary practice. The survey collected information on demographics, general health status, co-morbid medical conditions, and obstetric and gynecologic health. Quality of life was assessed using a modified Ladder of Life scale. Participants were asked about consistent gynecologic pain over the past six months, and those with chronic pain were asked to describe the location, nature, and exacerbating factors of their symptoms. The study population consisted of women previously seen by physicians at the University of Medicine and Dentistry of New Jersey-Robert Wood Johnson Medical School (UMDNJ-RWJMS).
Out of 4,872 mailed surveys, 36.8% were returned. The study population was predominantly Caucasian (83%) with an average age of 50.2 years.
The provided document does not contain specific recommendations or implications of the study.
In conclusion, the study found that the prevalence of vulvar pain was lower than previously reported in this particular survey. Chronic gynecologic pain, especially vulvar pain, significantly impacts both intimate and social aspects of quality of life. Self-reported stress and vaginal infections were identified as the strongest correlates of chronic vulvar pain.
How To Test For Vaginal Pain?
When you experience vaginal pain and decide it's time to seek answers, your doctor will become your most important ally. The diagnostic process usually starts with a thorough chat. Your doctor will ask you lots of questions about your symptoms: when they started, what they feel like, when they occur, what makes them better or worse, and your medical history. Don't hold back; every detail, no matter how small or embarrassing it might seem, can be a piece of the puzzle.
Common diagnostic steps include:
- Detailed Medical History: Discussion about symptoms, onset, triggers, and past health.
- Physical Examination: Gentle visual inspection of the vulva and vagina.
- Speculum Exam: To examine vaginal walls and cervix.
- Swabs: To test for infections (yeast, bacterial vaginosis, STIs).
- Bimanual Exam: To gently feel uterus and ovaries.
- Pelvic Floor Muscle Assessment: To check for tightness, tenderness, or weakness.
- Further Tests: Urine tests, blood tests, or imaging (like ultrasound) if needed.
(Read More: Navigating Vaginal Whitening)
Next comes a physical examination. This typically includes a gentle visual inspection of the vulva and vagina to look for redness, swelling, lesions, or discharge. A speculum exam, similar to a Pap test, might be done to examine the vaginal walls and cervix. During this, your doctor might take swabs to test for infections like yeast, bacterial vaginosis, or STIs. They might also perform a bimanual exam, where they gently feel your uterus and ovaries. In some cases, your doctor might also check your pelvic floor muscles to see if they are tight, tender, or weak. Depending on the findings, further tests might be needed, such as urine tests, blood tests (to check hormone levels or for inflammatory markers), or even imaging like an ultrasound if structural issues are suspected. The goal is always to get a clear picture of what's causing your discomfort so the right treatment can begin.
How To Cure Vaginal Pain?
The good news is that vaginal pain is often treatable, and while there might not always be a single "cure-all," a combination of approaches can provide significant relief and improve your quality of life. The path to relief really depends on the underlying cause. If it's an infection, targeted medication will likely clear it up. If it’s related to hormonal changes, hormone therapy or specific lubricants might be the answer. For muscle-related pain, therapies focusing on the pelvic floor are incredibly effective.
Sometimes, managing vaginal pain involves a multi-pronged approach, tackling different aspects of the issue simultaneously. This might mean addressing physical symptoms with medication or therapy, while also exploring lifestyle adjustments and even psychological support if stress or anxiety are playing a role. The "cure" isn't always about eliminating the pain entirely, but often about managing it effectively so you can live comfortably and fully. It's about finding the right tools and strategies that work for your unique situation.
(Read More: Oligomenorrhea: causes, symptoms, prevention, treatment)
Medicins For Vaginal Pain
When it comes to addressing vaginal pain, medicines can be a real game-changer, but the type of medicine depends entirely on the root cause. For infections, you might be prescribed antifungal creams or oral tablets for yeast infections, or antibiotics for bacterial vaginosis or STIs. If hormonal changes are causing dryness and pain, topical estrogen creams or rings can replenish moisture and restore tissue health.
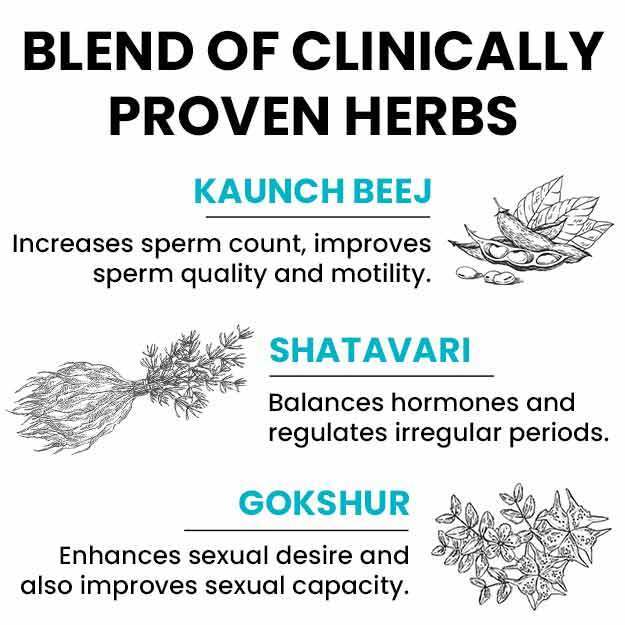
Types of medicines commonly used include:
- Antifungals: For yeast infections (creams, oral tablets).
- Antibiotics: For bacterial vaginosis or STIs (oral tablets, gels).
- Topical Estrogen: For hormonal dryness and atrophy (creams, rings).
- Nerve Pain Medications: Such as gabapentin or pregabalin, for nerve-related pain.
- Low-Dose Antidepressants: Can help modulate pain pathways.
- Over-the-Counter Pain Relievers: Ibuprofen, naproxen for general pain/inflammation.
- Topical Anesthetics: Lidocaine gels for localized numbing.
(Read More: Bleeding After Abortion: What to Expect and When to Get Help)
Surgery For Vaginal Pain
While many causes of vaginal pain can be managed with non-surgical methods, there are specific situations where surgery might be considered. It's typically seen as a last resort, reserved for cases where other treatments haven't provided relief or when there's a clear structural issue contributing to the pain. For instance, if severe endometriosis (where tissue similar to the lining of the uterus grows outside it) is causing deep pelvic and vaginal pain, surgery to remove these growths might be necessary.
Conditions that might warrant surgical consideration:
- Severe Endometriosis: To remove tissue growths causing pain.
- Vaginal Septum: Surgical correction of a tissue wall dividing the vagina.
- Severe Pelvic Organ Prolapse: To correct descending pelvic organs.
- Nerve Entrapment: Procedures to decompress or release an entrapped nerve in rare cases.
(Read More: Tubectomy Explained: Your Complete Guide)
Home remedies For Vaginal Pain
Sometimes, the simplest things can offer surprising relief from vaginal pain, especially when used in conjunction with medical treatments. Think of these as comfort measures that help soothe and manage discomfort in your daily life. A warm bath can be incredibly relaxing for tense pelvic muscles and can ease general soreness. You might want to add Epsom salts for extra soothing. Alternatively, a cool compress or an ice pack wrapped in a cloth applied to the external area can help numb pain and reduce inflammation.
Helpful home remedies include:
- Warm Baths: Relaxing for muscles and soothing general soreness.
- Cool Compresses/Ice Packs: To numb pain and reduce inflammation.
- Loose-Fitting, Breathable Clothing: Especially cotton underwear.
- Avoiding Irritants: Harsh soaps, perfumes, douches, scented hygiene products.
- Gentle Cleansing: Using pH-balanced cleansers or plain water.
- Water-Based Lubricants: For dryness, especially during intimacy.
(Read More: Bye-Bye Lines: Must Try Home Remedies for Stretch Marks)
Therapies For Vaginal Pain
Beyond medications, various therapies can play a vital role in addressing vaginal pain, especially when muscles, nerves, or psychological factors are involved. One of the most effective and commonly recommended is pelvic floor physical therapy. This is a specialized form of physical therapy where a trained therapist helps you learn to relax, strengthen, or coordinate your pelvic floor muscles. They might use techniques like manual therapy (gentle massage or pressure), biofeedback (using sensors to help you visualize muscle activity), and specific exercises. It's incredibly helpful for conditions like vaginismus, hypertonic (overly tight) pelvic floor muscles, or pain during intercourse.
(Read More: Tips on keeping your vagina healthy)
Counseling or psychological therapy can also be very beneficial. Chronic pain of any kind can take a toll on mental health, leading to anxiety, depression, and stress, which can, in turn, worsen pain perception. A therapist can help you develop coping strategies, manage stress, and address any emotional factors that might be contributing to your pain. Techniques like mindfulness, cognitive behavioral therapy (CBT), or acceptance and commitment therapy (ACT) can be powerful tools. Sometimes, chronic pain can make you feel isolated, and talking to a professional can provide much-needed support and guidance.
Tablets For Vaginal Pain
While we've touched on medications, it's worth specifically highlighting "tablets" as a form of treatment, which are orally administered medications that work systemically throughout your body. For infections, you might receive oral antifungal tablets for yeast infections or oral antibiotics for bacterial infections or STIs. For chronic nerve-related pain, specific tablets like gabapentin (Neurontin) or pregabalin (Lyrica) are often prescribed. These aren't traditional painkillers but work by calming overactive nerve signals.
(Read More: Vaginal Changes with Age: What to Expect and How to Adapt)
Sometimes, low-dose tricyclic antidepressants, like amitriptyline, are prescribed in tablet form, not for depression, but because they can help modify pain signals in the brain and reduce nerve pain. Over-the-counter pain relievers such as ibuprofen or naproxen are also available in tablet form and can help manage general inflammation and mild to moderate pain. Hormonal imbalances, especially in post-menopausal women causing vaginal atrophy, might sometimes be addressed with oral hormone replacement therapy tablets, though topical forms are often preferred for localized vaginal issues. The type of tablet prescribed will always depend on the specific diagnosis and your doctor's assessment.
Home Remedies For Vaginal Pain
Let's circle back to home remedies, as they are often the first line of defense and a constant source of comfort in managing vaginal pain. Beyond warm baths and loose clothing, consider these additional practical tips. Diet plays a role: some women find that reducing sugar intake, especially if recurrent yeast infections are an issue, can help. Probiotic-rich foods or supplements might also support a healthy vaginal microbiome, potentially preventing some infections. Staying well-hydrated is also generally good for overall health, including maintaining healthy mucous membranes.
(Read More: Vaginal burning: symptoms, causes, prevention, treatment)
Further home remedy considerations:
-
Dietary Adjustments: Reducing sugar intake, incorporating probiotics.
-
Hydration: Drinking plenty of water.
-
Product Choices: Avoiding harsh soaps, douches, and scented products.
-
Laundry Detergent: Using hypoallergenic, fragrance-free options for underwear.
-
Gentle Drying: Patting dry instead of rubbing after washing.
-
Natural Moisturizers: Applying pure, unscented petroleum jelly or coconut oil externally if dryness is a factor (check with doctor).
When it comes to personal care products, absolute simplicity is best. Avoid any douches, vaginal deodorants, bubble baths, or harsh soaps. Even some laundry detergents can be irritating, so opting for a hypoallergenic, fragrance-free detergent for your underwear might make a difference. After showering or bathing, gently pat the area dry instead of rubbing. Some women find relief by applying a thin layer of pure, unscented moisturizer (like a petroleum jelly or natural oil like coconut oil, if no allergies) to the external skin if dryness is a major factor, though always check with your doctor first. Remember, home remedies are fantastic for comfort and support, but they rarely replace the need for professional medical diagnosis and treatment, especially for persistent or severe pain.
(Read More: DIY Relief: Home Remedies for Managing Vaginal Pain)
Prognosis and complications
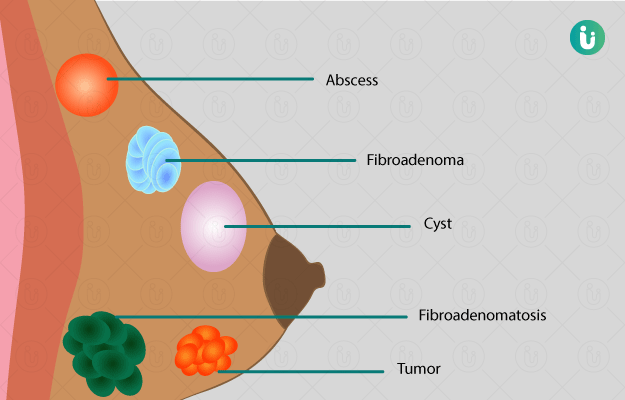
Vaginal pain is often unrelated to serious causes and is mostly self-limiting. Rarely, it may be related to vaginal fibroids or endometriosis, which may cause difficulty in the process of fertilisation and conception in the woman. In case of an ectopic pregnancy, a miscarriage is highly likely.
Risk of fatality due to vaginal pain is very low, and it holds an overall good prognosis. However, the quality of sex life of the woman is likely to be affected until pain lasts.
(Read more: How much water to drink in a day)
Prevention of vaginal pain
Since vaginal pain is caused due to several causes, its prevention can be done in many ways. Vaginal pain occurring during menstruation is inevitable if you have a family history. However, if disturbed menstruation is associated with an underlying disorder like polycystic ovarian syndrome (PCOS), you can get yourself treated. Maintaining a healthy lifestyle and weight will help you in the management of PCOD. You must, however, consult your gynaecologist for the best advice.
Vaginal pain during sexual intercourse can be prevented by using a lubricant, which will help to counteract vaginal dryness. Avoiding deep penetration during sex may help. Use of latex-free condoms can also help to avoid pain in allergics. Use of condom during sex will further help to avoid STI and eventually vaginal pain. Other ways in which vulvar infection can be avoided are:
-
Maintaining proper hygiene of the intimate area
-
Avoiding wearing tight synthetic clothing since bacterial growth occurs in warm, moist environment (this will also help in avoiding allergy to clothings)
-
Drinking enough water to prevent UTI
-
Avoiding the use of cleansers and other scented products on the vagina
-
Avoiding washing too often, since it will wash away the good bacteria
-
Changing underwears every day
Avoiding the use of uterine contraceptives can also help in preventing vaginal pain.
During pregnancy, vaginal pain can be prevented by avoiding smoking, which increases the risk of ectopic pregnancies. Taking care of general health and hygiene is also important to avoid vaginal infections.
Read more: Treatment of vaginal bleeding
Summary
This article comprehensively covers vaginal pain, defining it as any discomfort in the vaginal area. It identifies diverse causes including infections (yeast, bacterial, STIs), skin conditions, muscle problems (pelvic floor dysfunction), nerve issues, hormonal changes, and psychological factors. Symptoms range from burning and stinging to aching and throbbing, often triggered by activities like intercourse or prolonged sitting. Diagnosis involves medical history, physical exams, and tests for infections. Treatment varies by cause and includes medications (antifungals, antibiotics, hormonal therapies, nerve pain meds), physical therapy, counseling, and, in rare cases, surgery. Home remedies like warm baths and loose clothing offer comfort. While prognosis is generally good, prevention focuses on hygiene, avoiding irritants, and lifestyle adjustments.
References
- American College of Obstetricians and Gynecologists [Internet] Washington, DC; Dysmenorrhea: Painful Periods
- American Pregnancy Association. [Internet]; Stages Of Childbirth: Stage I.
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Period pain: Overview. 2008 Feb 22 [Updated 2016 Jul 1].
- Better health channel. Department of Health and Human Services [internet]. State government of Victoria; Menstruation - pain (dysmenorrhoea)
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Diary: Premenstrual syndrome (PMS). 2017 Jun 14.
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Endometriosis: Overview. 2008 Feb 25 [Updated 2017 Oct 19].
- UCLA Health. What are Fibroids. California, United States [Internet]
- Office on Women's Health [Internet] U.S. Department of Health and Human Services; Pelvic inflammatory disease.
- National Center for Advancing and Translational Sciences. Adenomyosis. Genetic and Rare Diseases Information Center
- Government of Western Australia. Ectopic pregnancy. Department of Health
- MedlinePlus Medical Encyclopedia: US National Library of Medicine; Ectopic pregnancy
- National Cancer Institute [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Gestational Trophoblastic Disease Treatment
- Office on Women's Health [Internet] U.S. Department of Health and Human Services; Vaginal infections.
- F. A. Taran, E. A. Stewart, S. Brucker. Adenomyosis: Epidemiology, Risk Factors, Clinical Phenotype and Surgical and Interventional Alternatives to Hysterectomy. Geburtshilfe Frauenheilkd. 2013 Sep; 73(9): 924–931. PMID: 24771944
- Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995-. Dyspareunia and quality of sex life after surgical excision of endometriosis: a systematic review.